Developing and testing new approaches for meeting patient needs for virtual medicine
Challenge
The Lab at OPM partnered with a new design team from the Veteran’s Experience Office to look at the adoption of telehealth during the COVID-19 pandemic and identify how to best leverage the technology for the benefits of veterans and their caretakers. We conducted an extensive research phase that included analysis of Voice of the Customer feedback and qualitative interviews with patients and care teams. That research identified some key “moments that matter” for a positive patient experience of telehealth. For first-time telehealth users, these moments can mean the difference between becoming an enthusiastic adopter or a reluctant and frustrated patient. By contrast, recovering from negative initial experiences and rebuilding Veteran confidence in the telehealth modality proved difficult. Our challenge in moving from research to action was to develop tools and practices that best positioned VHA providers and care teams to meet these key moments in a new telehealth patient’s journey.
Process
As part of our research we identified high-performing care teams that were delivering positive telehealth experiences. Through a series of co-design workshops with some of these teams, we developed several concepts to help care teams think though the key touchpoints for new telehealth patients and ensure they were taking a patient-centered approach to offering telehealth.
Our first prototype was for a new training workshop that would teach care teams the moments that matter for patients and enable them to brainstorm how they would address them as a team. Our goal was not to offer top down solutions but instead give the team space to align on their approach to telehealth scheduling and onboarding. However, in piloting these workshops we observed several issues. First, getting the entire care team scheduled for a training would be extremely challening. Second, the nurses and support staff immediately deferred to the doctor or the facilitator in the workshop, reducing the ability to hear diverse perspectives and learn from each other. Finally, the workshop went into too much detail and would be difficult for staff to take away clear actions.
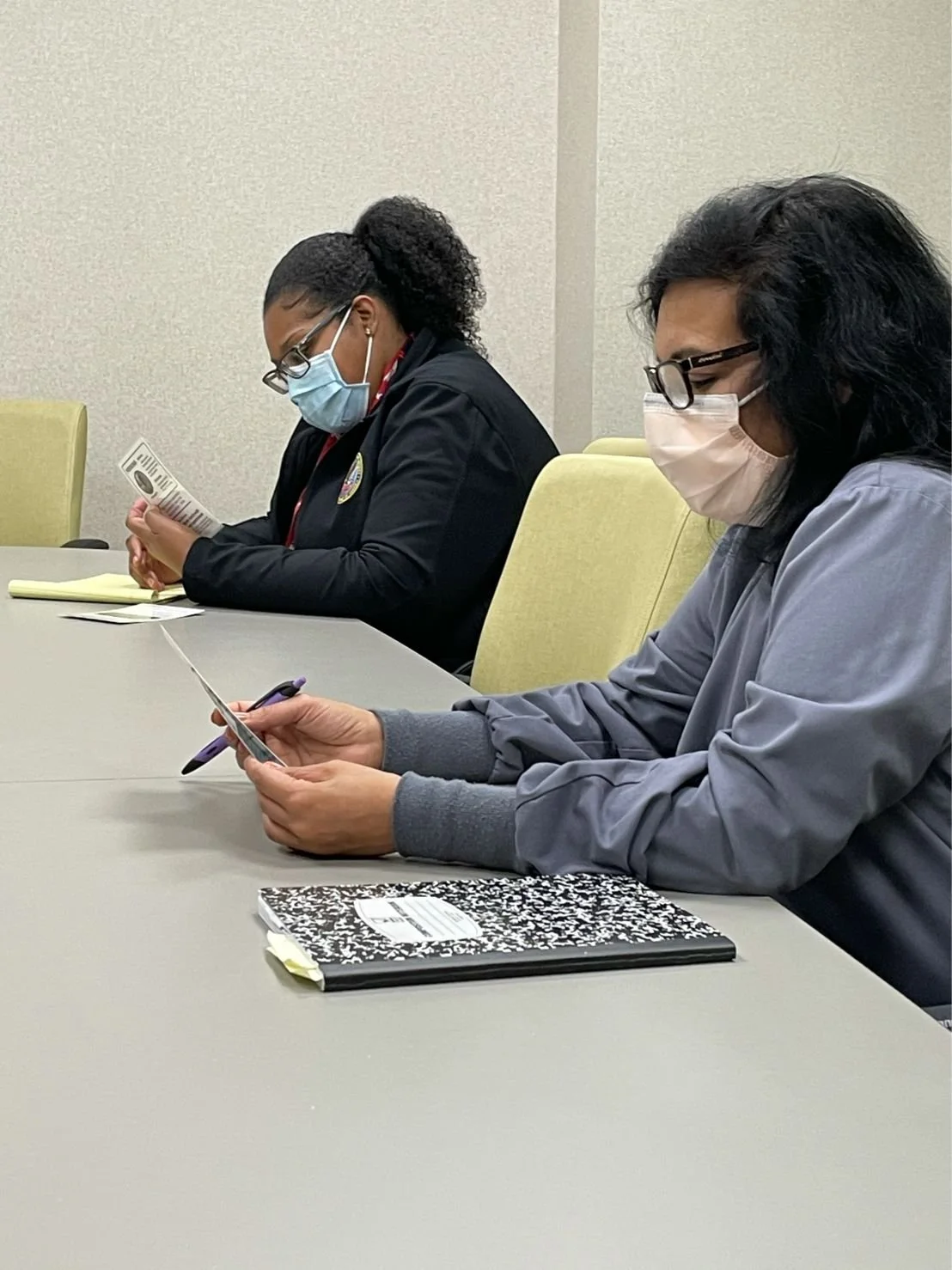
So we pivoted and revised the training into a new tool we called the “Huddle Challenge” - a simple role playing activity that care teams could integrate into their existing daily stand-up routine. The goal was for care teams to take on personas of typical telehealth patients and role-play the scheduling and onboarding process. Other members of the team were able to observe and provide feedback. In one activity, the care teams printed out the scheduling email that patients received and reviewed it as a team. This was the first time most members of the team had ever read the email, and they instantly gained empathy for why patients might be confused about telehealth appointments.
Outcome
We piloted the Huddle Challenge with a few teams in different VHA locations. Care teams enjoyed the opportunity for peer-based learning and also appreciated the efficiency of the exercise, as it was easy to work into the existing schedules. We made slight revisions to emphasize the peer feedback component and simplify the activities, and then the VEO team worked with a regional office to build out additional cards and to scale the pilot more broadly.
This and other efforts based on our research have helped contribute to increased usage and satisfaction with telehealth among VHA patients.
“91.8% of Veterans who have used telehealth are satisfied with the services, and 89% report trusting it as part of their overall healthcare”
Project team: Toni Hightower, Todd Tinius, Rich Dumancas, Kathy Casino, Eric Faulkner, Karen Cutright, Jennifer Gardner, Lisette Baylor, Roseann Stempinski, and James Gasapo